Wear me because I am the most important commodity in the world in recent times who can save lives.
I became essential commodity before and after the World Health Organization (WHO) declared a global health emergency (COVID-19) on January, 30th, 2020.
Face mask as my name, had higher price of 166% than the 90-day average price according to the consumer advocacy organization report cited in usatoday.com
I was placed under essential commodities Act by the Government of India up to 30/06/2020 and now an important commodity internationally.

This shows how powerful I am. Do you know why you must wear me? I know you are thinking about the answer but simply, you have to save your life and others you love so much. Your next life on the earth is determined by me.
Wear me because I protect you against Small and large droplets (through sneezing, coughing and/or talking).
Wear me to protect your loved ones from getting infected from you knowingly (symptomatic) or unknowingly (asymptotic/carrier).

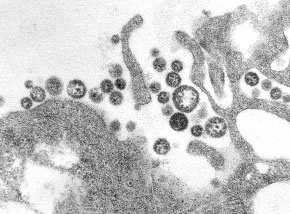
Wear me (face mask) to slow down the spread of the virus we cannot see with our naked eyes since we want to move. We know when we move, the virus moves so please wear me to reduce the infections to save you and me, our loved ones and the community.
Wear me because it has become necessary that recent studies from NHK world, Japan with a documentary titled; fighting a Pandemic showed that the virus can travel through micro droplets ( can only see the virus in the droplets with the aid of microscope). And much micro droplets are produced when an infected person talks loud but when you wear me, it will protect you against this situation.
Wear me to save your life. Wear me to save your beloved ones. Wear me to save the community cos we need everyone alive including you to build this nation together. It is your responsibility, my responsibility, our responsibility and the nation’s responsibility.
How do you wear and remove me (face mask)?

What must you know before wearing me (face mask)?
1. Check especially the cloth face mask if it has at least three (3) layers of fabric before wearing me.
2. Also, observe if the inner layer that will touch the nose and mouth has unprinted fabric to prevent you from skin allergies and others.
3. Observe if there is no holes in me before wearing me.
4. Check if I will be able to fit snugly but comfortably against the side of the face before wearing me.
5. I should have ties or ear loops for securing.
6. I should also have breathability.
7. Especially the cloth face mask, it should be washable for reuse.
Kindly wear me because you’re all potential COVID-19 until tested to know your status. Again, wear me because you or me or we may be asymptomatic ( carriers) who can infect others unknowingly. You are wearing me not to feel comfort but there is a need to do so for your own safety, my safety, our safety and the community’s safety .
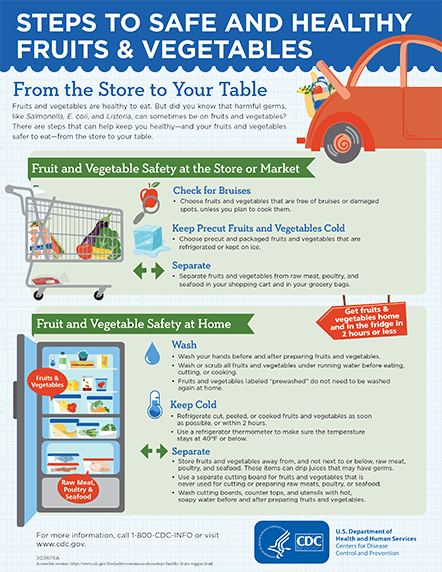
Continue to wash your hands with soap under running water regularly or apply alcohol based 70% hand sanitiser as you wear me (face mask).
#Don’tbethespread
#staysafe
#wearmeifyoumove
Sources.
1. https://www.cdc.gov>2019-ncov
2. https://www.who.int>diseases>wh…
3. https://www.webmd.com>lung>c…
4. https://www.theguardian.com